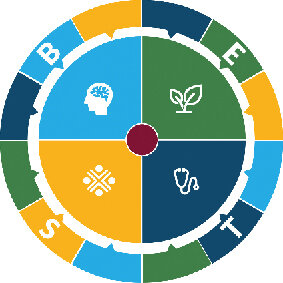
The BEST Framework
The term “Neglected Tropical Diseases” was coined in 2003, to bring together a concerted global effort. Addressing NTDs under a single ‘brand’ has significantly added to the interest in NTDs, and subsequently added to funding and implementation support. This briefing outlines why the BEST framework for NTDs is needed and what it seeks to achieve. It calls on NTD stakeholders to adopt the BEST framework and embed cross-sectoral approaches and systems thinking in their work.
The progress made since 2003 masks gaps between ‘priority’ and ‘other’ NTDs, between disease control/elimination efforts and care programmes, between medical and environmental/behavioural interventions and between the core NTDs community and other important stakeholders that are not routinely or systematically engaged in technical and advocacy discussions. Certain sectors such as vector control, veterinary public health, care programmes and WASH are underrepresented in NTD coalitions, conferences and national action plans.
These gaps make the NTD community less able to plan, fund and deliver a comprehensive and inclusive approach that effectively targets the population groups most in need, to use programme resources effectively and to mobilise further resources and efforts from other relevant sectors and programmes.
SDG target 3.3 ensured representation of NTDs in the post-2015 Sustainable Development Goals (SDGs). The SDGs mark a new agenda for inclusive, equitable and sustainable development, including universal access to key services. The commitment embodied in the SDGs to leave no one behind recognises the need for cross-sectoral action to build strong systems and ensure equitable access across health and other sectors to sustain programme efforts to control and eliminate NTDs. Investment in health system strengthening is critical to realise this vision and improve health and other outcomes.
While the term ‘NTDs’ usefully groups diseases together for advocacy and resource allocation purposes, it does not define the breadth of programme interventions needed to address them. The BEST framework gathers the diverse cross-sectoral efforts needed to reach control, elimination and eradication targets for NTDs. It sets out the NTD community’s commitment to forging new partnerships and working across sectors to ensure equity and inclusion. It complements existing frameworks such as the WHO NTD Roadmap and the WASH and NTDs strategy, the UN Convention on the Rights of Persons with Disabilities, Community Based Rehabilitation, WHO ICF, and other initiatives to achieve Universal Health Coverage and the Sustainable Development Goals.
Rationale for a new comprehensive framework for NTDs:

Clearer message – stronger advocacy: a conceptual framework that includes all NTD interventions can generate further political and financial momentum for NTDs. It increases the potential for success of NTDs programmes by moving away from a narrow disease-control and primarily treatment-focused approach and makes it easier to demonstrate the value of NTDs to systems strengthening and the contribution of NTDs efforts to Universal Health Coverage.
Joint framework – improved integration: a clear framework for action justifies collaboration between different programmes and sectors, without the need to modify institutional structures.
Comprehensive framework – rationalised funding and programmes structures: the BEST framework can provide a standardised approach for a set of comprehensive NTD interventions. This will encourage consistency and coherence across NTD programmes and provide a clear structure through which NTD investments can be made and results can be measured by NTD partners and endemic country governments. This will also engage relevant sectors with appropriate expertise are engaged.
Behaviour

Behaviours play a key role in successfully tackling NTDs. Physical behaviours have long been addressed in many NTDs programmes, tackling aspects such as personal hygiene and other risk-reducing behaviours. Programmes could be further strengthened by emphasising aspects relating to vector control, waste management and livestock keeping, as well as addressing uptake of protective and treatment-seeking behaviours.
Other behaviours, however, are often ignored or under-prioritised in NTD programme design. Addressing attitudes at all levels including community, schools, the health systems etc., can contribute greatly to the success of programmes by promoting inclusion by families and society of people affected by NTDs, particularly those subjected to stigma and misconception.
Institutional behaviours are necessary to ensure NTD programmes contribute to system strengthening and the progressive achievement of UHC; examples include collaborative programme design across sectors and agencies to fund, develop and implement comprehensive NTDs programmes.
Environment

Environmental measures for disease control are often only partially incorporated into NTD programmes or delivered separately from and without consideration for disease control priorities. While some NTD programmes include environmental sanitation aspects by encouraging the construction of basic household latrines, a comprehensive approach to environmental sanitation is needed to achieve disease control objectives by safely separating waste from humans and animals and reduce the risk of vector breeding and contamination of water and soil.
In healthcare settings, this must include Infection Prevention and Control and vector control measures. Safe, reliable, affordable, universally accessible and sustainable water infrastructure is also needed to prevent consumption of contaminated water, reduce contact with surface water and enable personal hygiene practices.
A robust approach to environmental disease control must also include the use of Integrated Vector Management. Additionally, Veterinary Public Health services should be incorporated within disease control efforts, ensuring appropriate livestock keeping and food safety practices and utilizing the available expertise for disease surveillance and control.
Social Inclusion

Driving progress towards Universal Health Coverage by strengthening health systems to deliver essential quality health services and prioritising coverage of populations at risk of NTDs is a critical step towards equity and inclusion. Progress towards social inclusion and equity can only be achieved by addressing barriers to participation in a person’s environment, improving universal access to quality promotive, preventive, curative and rehabilitative services and ensuring poverty is not a barrier to accessing NTD services in line with UHC.
This requires mainstreaming inclusion across all NTD interventions, ensuring infrastructure is accessible and support services reach women, children, people with disabilities and other targeted population groups.
Empowerment of communities affected by NTDs is necessary to facilitate greater agency, participation and support of all individuals and communities to make decisions about services for their health and wellbeing.
Addressing stigma and discrimination against people affected by NTDs will mean the provision of high-quality social support services in the family and the community, and formal and informal work.
Treatment and care

Achieving progress towards Universal Health Coverage means strengthening health and other systems so they are equipped to deliver a comprehensive treatment. This is based on a continuum of care approach that goes beyond efforts to prevent or cure an infection, by responding to the broader needs of individuals and communities.
Preventive chemotherapy is a fundamental component of NTD programmes and should be implemented where a clear strategy for treatment has been developed and where tools and safe and effective drugs enable implementation of large-scale treatment alongside other BEST interventions. A comprehensive approach to NTDs must also ensure that sufficient capacity for surgery within the national health system is sustained. Diseases management and self-care are essential for reducing the severity of many diseases, to prevent suffering and increased vulnerability to poverty, stigma and exclusion.
Access to quality, affordable rehabilitation services not only respects human rights but can deliver economic and social benefits, for example by facilitating recovery from surgery, addressing pain management and maintaining dignity and maximising independence. As diseases decrease their burden and elimination is achieved, a functional disease surveillance system is essential, to ensure that achieved goals are maintained via a strengthened health structure capable of detecting disease outbreaks and potential re-emergence.